Colitis is an inflammation of the colon and can emerge in diverse forms. Some types of colitis may result in a life-threatening condition, so it is vital to diagnose the type of colitis affecting you since treatment varies for each.
Collagenous colitis is a rare type of bowel inflammation affecting the colon and is characterized by persistent non-bloody diarrhea and abdominal pain or cramps. Adults aged 50 and above are more likely to develop this condition than other age groups.
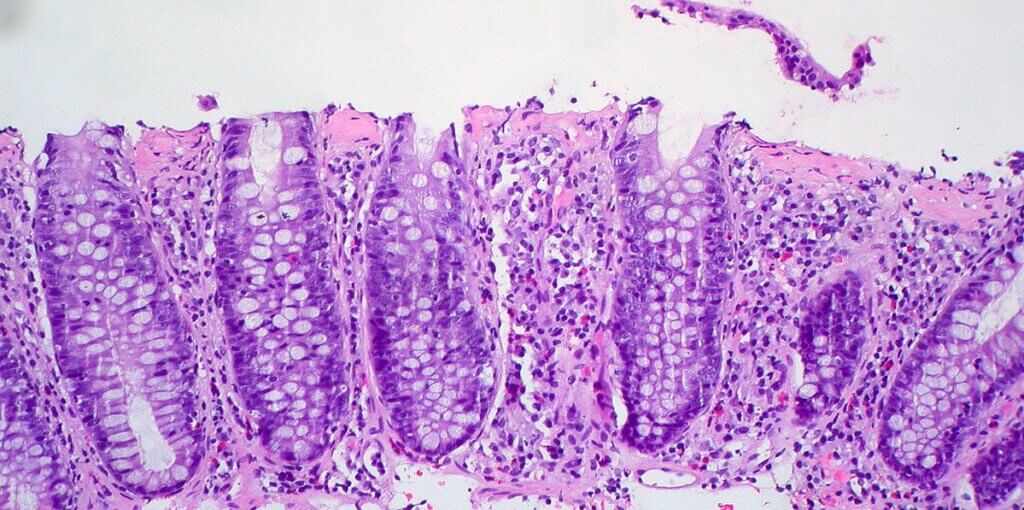
Researchers categorize collagenous colitis as one of the two types of microscopic colitis because inflammation on the outer surface of the colon is not visible when examined through a colonoscopy or sigmoidoscopy. But visible when a biopsy goes under a microscope.
Cause of Collagenous Colitis
While researchers are still unsure of the exact cause of collagenous colitis, several studies have shown that collagenous colitis can be caused by genetic and environmental factors.
It also occurs when the immune system attacks bacteria in the colon.
Several pieces of research suggest that the intake of certain medications such as proton pump inhibitors and Nonsteroidal anti-inflammatory drugs (NSAIDs) can trigger the development of collagenous colitis. However, there is no consistent data to support this claim.
Researchers also suggest that women are more likely to be affected by this disease than men. An elevated estrogen level in women contributes to the high disparity between both genders.
While gluten, a protein found in products like wheat, oat, and barley, is not the actual cause of microscopic colitis, it could trigger the inflammation of the colon.
Symptoms of Collagenous Colitis
It is common for collagenous colitis patients to experience diarrhea and abdominal pain; however, the severity and duration vary according to each individual.
You may experience mild discomfort, while a loved one may experience disabling symptoms. Other symptoms of collagenous colitis include:
- The feeling of bowel movement
- Inflammation, infection, chills, and fever.
- Constant pain
- Abdominal pain occurring in waves
- Bloating
- Flatulence
Collagenous and lymphocytic cases that do not respond to medication may require surgery to remove all or part of the colon.
Diagnosis
Diagnosis is the first step to treating collagenous colitis. A gastroenterologist will perform a physical examination and ask questions about your lifestyle habits, medical history, medication, and eating patterns.
For an accurate diagnosis, your doctor will take different biopsies from a separate section of your colon to examine under a microscope.
When in doubt, your doctor may order additional tests such as CT scans, MRIs, blood and stool tests to ascertain if another underlying gastrointestinal condition causes your condition.
Treatment
To treat microscopic colitis, the first thing you should do is change your diet. Your doctor may advise you to eat low-fat food and avoid foods rich in gluten to help relieve diarrhea.
Your doctor may introduce good bacteria known as lactobacilli to replace immunogenic strains of bacteria that may be responsible for collagenous colitis.
Your doctor may prescribe antidiarrheal medication such as loperamide (Imodium) or bismuth subsalicylate (Pepto-Bismol) to reduce discomfort. Your doctor may discontinue the use of medicine as a treatment option if your symptoms persist or worsen.
Surgery
In severe cases, medications may not effectively treat collagenous colitis; your doctor may suggest surgery to remove all or part of your color. However, surgery may not be necessary for collagenous colitis.
Home Remedies
If you experience collagenous colitis, drinking excess water is key to curing this condition. With each bowel movement, you may lose a significant amount of fluid. So adequate fluid intake is crucial to maintaining balance, or it may lead to dehydration, abdominal pain, and cramping.
Eat easily digestible food such as rice, applesauce, and vegetables. Avoid beverages rich in sugar, alcohol, and caffeine that may trigger colitis. You can slowly add fiber back to your diet if symptoms improve.
Avoid spicy food, fried and fatty food. Consistently eating small meals instead of one large meal may help heal faster and relieve diarrhea.
While the risk of death or developing colon cancer is relatively low with collagenous colitis, your doctor may test for other conditions with the symptoms you are experiencing if your state doesn’t improve after exhausted all options. Always remember that eating healthy is the key to living your best life.