If you searched “what causes heart failure”, you’re probably trying to connect dots: “Is it my blood pressure? That old heart issue? My breathing problems? Something else?”
Here’s the straight answer we give patients in real life:
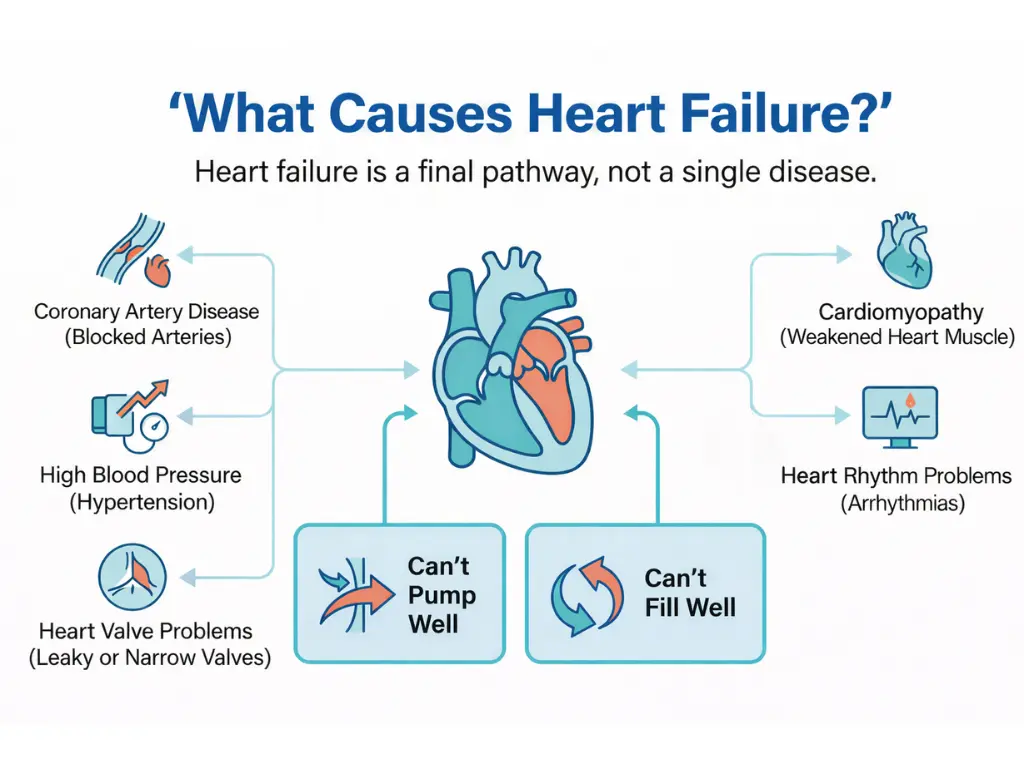
Heart failure isn’t a single disease. It’s a final pathway—a situation where the heart can’t keep up with what the body needs. That can happen because the heart muscle gets weaker, stiffer, or it’s dealing with too much pressure/volume over time. The key is this: most heart failure has an underlying cause we can look for and treat.
What heart failure really means
Heart failure doesn’t mean the heart “stops.” It means:
- The heart can’t pump effectively, or
- The heart can’t fill effectively, or
- Both
When that happens, the body may start to “back up” with fluid and/or struggle to deliver oxygen where it’s needed—especially during activity, infections, stress, or dehydration.
People often ask “what causes congestive heart failure?” Clinically, “congestive” is often used when fluid buildup is part of the picture (swelling, lung congestion). Many people use “CHF” to mean heart failure in general.
A quick, real-world example (anonymous and non-diagnostic)
We’ll keep this anonymous, but it’s a common scenario:
A patient in their 40s–60s notices they’re getting winded walking from the car to the store. They think it’s “just getting older” or “being out of shape.” Then swelling shows up around the ankles after long days. They also mention they’ve had high blood pressure “for years,” but it hasn’t always been under control.
That pattern matters because long-term high blood pressure is one of the most common reasons the heart gradually becomes strained—often quietly—until symptoms show up.
This isn’t a diagnosis. It’s just how heart failure sometimes enters the room.
The most common causes of heart failure
When we evaluate heart failure, we usually think in buckets. Many patients have more than one cause at the same time.
1) Coronary artery disease and heart attacks
If the heart’s own blood supply is reduced (coronary artery disease), the heart muscle may become damaged over time—or suddenly during a heart attack.
- Scarred or injured heart muscle can weaken pumping.
- Reduced blood flow can contribute to heart rhythm problems and progressive strain.
Common patient question: “Can heart failure come from clogged arteries?”
Yes—coronary artery disease is a major contributor.
2) High blood pressure (hypertension)
A very common question we hear is: “Does hypertension cause heart failure?”
It can.
When blood pressure stays high over time, the heart has to pump “uphill” constantly. That extra workload can lead to:
- Thickening of the heart muscle (stiffness)
- Reduced ability to fill normally
- Eventual weakening in some cases
uncontrolled blood pressure can slowly “wear the heart down.”
3) Heart valve problems
Heart valves act like one-way doors. If a valve is too tight (stenosis) or too leaky (regurgitation), the heart has to work harder.
Over time, valve disease can lead to heart failure because the heart is:
- Pumping against abnormal resistance, or
- Handling too much volume returning backward
4) Irregular heart rhythms (including AFib)
Another very common search: “does afib cause heart failure?” / “can afib cause heart failure?”
It can—especially if the heart rate stays too fast for too long or if the rhythm problem worsens how efficiently the heart fills and pumps.
AFib (atrial fibrillation) is an irregular rhythm that can:
- Reduce efficient filling (“atrial kick” is lost)
- Trigger persistently fast heart rates in some people
- Increase strain on the heart over time
heart failure and AFib often travel together—either one can make the other more likely, depending on the person.
5) Cardiomyopathy (weak or stiff heart muscle for different reasons)
“Cardiomyopathy” just means the heart muscle is abnormal. Causes can include:
- Inherited (genetic) conditions
- Prior viral inflammation of the heart (myocarditis)
- Alcohol-related damage
- Some chemotherapy or medication-related effects
- Long-standing uncontrolled blood pressure
This bucket matters because the treatment approach can differ depending on the specific cause.
6) Diabetes, obesity, sleep apnea, and metabolic strain
These are not “one event” causes. They’re systems-level stressors that raise heart failure risk over years by contributing to:
- High blood pressure
- Vascular disease
- Inflammation and metabolic load
- Rhythm issues
You’ll notice a theme: these conditions often cluster together, and the combined effect can be bigger than any one factor alone.
7) Lung pressure problems and right-sided heart failure
People also search “what causes right sided heart failure”—and that’s an excellent question.
Most right-sided heart failure develops because the left side struggles first. But right-sided failure can also come from problems that raise pressure in the lungs, such as:
- High blood pressure in the lungs (pulmonary hypertension)
- Pulmonary embolism (a blood clot in the lungs)
- Lung diseases such as COPD
Right-sided failure often shows up with:
- Swelling in legs/ankles
- Abdominal bloating or fullness
- Weight gain from fluid
- Shortness of breath (often overlaps with lung symptoms)
8) Acute triggers that can “unmask” heart failure
Sometimes heart failure has been building quietly—and then something tips the body over, such as:
- Respiratory infections
- Significant stress on the body
- Uncontrolled blood pressure spikes
- New rhythm problems
- Blood clots in the lungs
This is why someone can feel “fine-ish” and then feel dramatically worse within a short window.
What causes heart failure in young adults (and why we take it seriously)
If you’re searching “what causes heart failure in young adults”, it’s understandable to feel alarmed.
Heart failure is less common in younger people, but when it happens we think about causes like:
- Inherited cardiomyopathy
- Myocarditis (heart inflammation), sometimes after viral illness
- Rhythm-related cardiomyopathy (heart rate too fast too long)
- Congenital or structural heart conditions
- Substance-related causes (stimulants, heavy alcohol use, certain drugs)
In younger adults, the “why” matters a lot—because some causes are treatable and reversible when caught early.
How we figure out the cause (diagnosis without guesswork)
Patients often want a single test that “proves” the cause. In real ER medicine, it’s usually a combination of:
- A careful symptom story (what changed, how fast, what triggers it)
- Physical exam (fluid signs, lung sounds, circulation clues)
- Heart rhythm testing (like an ECG/EKG)
- Imaging (often a chest X-ray; sometimes more depending on symptoms)
- Ultrasound of the heart (echocardiogram) to look at function and structure
- Lab testing that helps us assess strain, oxygenation, kidney/liver impact, and possible triggers
We stay careful here: we don’t guess—we follow the pattern of symptoms + exam + tests.
Treatment depends on the cause (and the goal is stability + safety)
If you’ve read generic articles, they often sound vague here. Let’s make it practical:
Treatment has two goals:
- Help you breathe and feel better, and reduce fluid overload if present
- Treat the driver (the cause) and reduce future strain
Depending on what’s going on, that can involve:
- Medications that help the body shed excess fluid (when appropriate)
- Blood pressure support and control
- Rhythm management when an irregular rhythm is part of the problem
- Treatment for coronary disease if that’s in the picture
- Targeted treatment if lung disease or a pulmonary embolism is suspected
- Coordinated follow-up and long-term management
You don’t need to memorize treatment lists. You do need to know when symptoms are serious enough that waiting isn’t worth the risk.
Warning symptoms that shouldn’t wait
If you’re experiencing any of the following, it’s reasonable to treat it as urgent—especially if symptoms are new, rapidly worsening, or feel different than your baseline:
- Chest pressure, tightness, or pain (especially with sweating, nausea, or shortness of breath)
- Severe shortness of breath at rest, or struggling to speak full sentences
- Fainting, near-fainting, or new severe dizziness
- Blue/gray lips or face, or severe confusion
- A racing heartbeat that doesn’t settle, or new irregular heartbeat with weakness
- New swelling that’s rapidly getting worse, especially with breathing difficulty
- Coughing up pink/frothy sputum or severe breathlessness that feels sudden
- Any symptom pattern that makes you think: “something is wrong right now”
If you’re experiencing shortness of breath, chest pressure, swelling, or a fast/irregular heartbeat—and you’re in or near Angleton or Brazoria County—it’s reasonable to get evaluated rather than trying to tough it out at home. If it turns out not to be heart failure, that’s still a win: you got checked and you’re safer for it.
Angleton ER is open 24/7, and we have on-site diagnostics (including lab testing and imaging) to help assess urgent symptoms when time matters.
Frequently Asked Questions
What can cause heart failure?
Most often, heart failure is caused by another condition that damages or strains the heart over time—commonly coronary artery disease, high blood pressure, valve disease, irregular rhythms, or cardiomyopathy.
What causes congestive heart failure (CHF)?
“CHF” is often used to describe heart failure when fluid congestion is part of the picture (like lung congestion or swelling). The underlying causes are similar: blood pressure strain, coronary disease, valve disease, rhythm problems, cardiomyopathy, and sometimes lung-related strain.
Does hypertension cause heart failure?
Long-term uncontrolled high blood pressure can contribute to heart failure by making the heart work harder over time, which can lead to stiffness, thickening, and eventually reduced function.
Can AFib cause heart failure?
AFib can contribute to heart failure—especially when the heart rate stays too fast for too long or when the rhythm reduces the heart’s efficiency. It’s also common for AFib and heart failure to coexist and worsen each other.
Can COPD cause heart failure?
COPD and other lung diseases can contribute to right-sided heart failure, particularly when lung disease raises pressure in the pulmonary circulation and forces the right side of the heart to work harder.
What causes right sided heart failure?
Most commonly, left-sided heart failure leads to right-sided failure over time. Right-sided failure can also be caused by high pressure in the lungs, pulmonary embolism, or lung diseases such as COPD.
Educational only. This is not medical advice or a diagnosis. If symptoms are severe, rapidly worsening, or you’re concerned, seek in-person evaluation.