If you searched “what are the 4 stages of congestive heart failure,” you’re probably trying to do something very human:
You’re trying to understand what’s happening—without spiraling.
Let’s slow it down and make it practical.
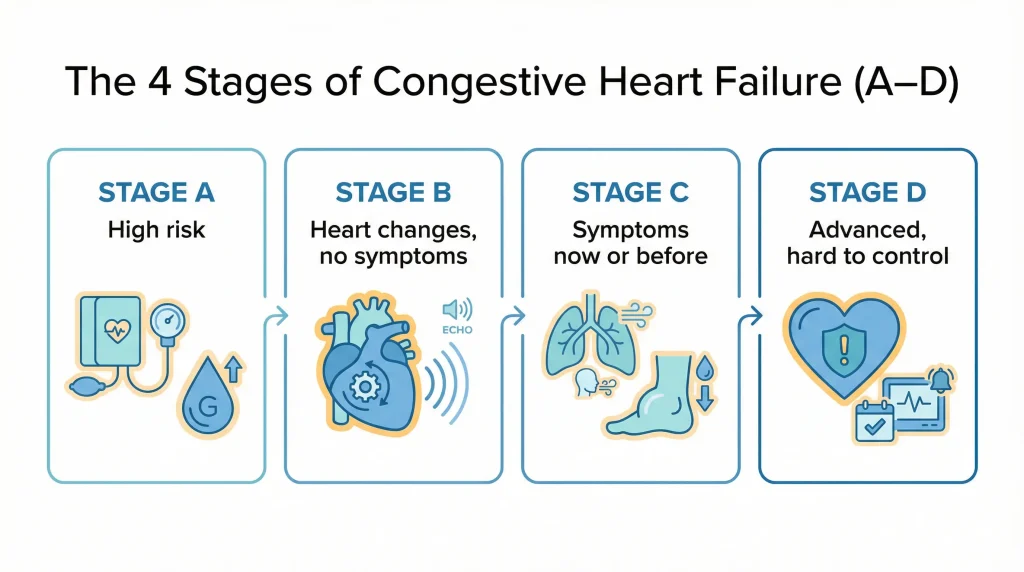
When doctors talk about “stages,” we’re usually referring to a 4-stage system (A–D) that helps describe risk, heart changes, and symptoms over time. It’s not meant to scare you. It’s meant to guide decisions—what to monitor, what to treat, and how urgently to act if symptoms change.
Educational only. This is not medical advice or a diagnosis. If symptoms are severe, rapidly worsening, or you’re concerned, seek in-person evaluation.
A quick anonymous scenario
Someone comes in from Angleton/Brazoria County and says:
- “I’m not collapsing… but I’m more winded than I used to be.”
- “My ankles are swelling by evening.”
- “I’m sleeping propped up.”
- “I keep telling myself it’s stress or getting older—but it’s getting worse.”
They’re not looking for a label. They’re looking for clarity:
Is this something I can watch… or something I shouldn’t ignore?
That’s exactly what staging is supposed to help with.
what “CHF” and “heart failure” actually mean
Heart failure doesn’t mean your heart “stopped.” It means your heart isn’t pumping or filling as effectively as your body needs.
“Congestive” is commonly used when fluid backup (congestion) is part of the picture—like fluid in the lungs or swelling in the legs.
The 4 stages of congestive heart failure (the A–D system)
People often call these “Stage 1–4,” but in most medical settings you’ll hear them as Stage A, B, C, and D.
Stage A: High risk — but no heart damage and no symptoms
This stage means:
- You may have risk factors (like high blood pressure, diabetes, coronary artery disease, obesity, smoking history, or a strong family history)
- No known structural heart changes
- No heart failure symptoms
What it can feel like:
Often… it feels like nothing. And that’s the point—this is where prevention matters most.
What typically helps at this stage (big picture):
- Treating risk factors consistently
- Lifestyle changes that are sustainable (not extreme)
Stage B: Heart changes are present — but no heart failure symptoms yet
This stage means:
- There’s evidence of heart structure/function changes (your clinician might see this on imaging like an echocardiogram)
- But you don’t have heart failure symptoms
What it can feel like:
Still may feel normal day-to-day.
Why this stage matters:
This is often the window where good medical follow-up can delay or prevent symptoms later.
Stage C: Heart changes + symptoms (now or in the past)
Stage C means:
- Heart changes are present and
- You have current symptoms or you’ve had symptoms before
This is where many people first realize: “Okay—this is real.”
What it can feel like (real-life language):
- Getting winded doing normal activities
- Needing more breaks than usual
- Swelling in ankles/legs
- A cough or “chest congestion” that doesn’t behave like a typical cold
- Sleeping propped up because lying flat feels worse
- A noticeable drop in stamina that feels out of proportion
Stage C includes current OR previous symptoms—so even if you’re feeling better today, your medical team may still refer to Stage C if you’ve had symptom episodes before.
Stage D: Advanced heart failure — symptoms are difficult to control
Stage D means:
- Heart failure is advanced and
- Symptoms can be severe, frequent, or hard to manage despite treatment
- People may need specialized therapies and close follow-up
What it can feel like:
- Shortness of breath with minimal activity—or sometimes even at rest
- Frequent flare-ups of swelling/fluid overload
- Very limited stamina
- More urgent visits or hospitalizations
This is the stage that makes people ask the hardest questions. If that’s you, we want you to hear this clearly:
Stage D is not a verdict. It’s a way to signal that your care may need to be more specialized and more tightly managed.
“Stages” vs “Classes”
You’ll also see “Classes I–IV” online. That’s usually the NYHA functional classification, which is a different system.
Here’s the simplest way to think about it:
- Stages (A–D) describe risk and heart disease progression
- Classes (I–IV) describe how limited you feel by symptoms right now
Quick cheat sheet (NYHA classes):
- Class I: No symptoms with normal activity
- Class II: Symptoms with more-than-usual exertion (some limitation)
- Class III: Symptoms with minimal activity (marked limitation)
- Class IV: Symptoms even at rest
A person can be Stage C (because they’ve had symptoms) but be Class II on a good month and Class III during a flare. That’s one reason you’ll see different “labels” at different times.
How doctors actually use staging
When staging is used well, it helps guide:
- How closely you should be followed
- What kinds of medications or therapies might be considered
- Whether we’re focusing on risk reduction, symptom control, or advanced management
- How seriously we take symptom changes (especially breathing changes)
What staging should not do:
- It should not be used as a “countdown clock.”
- It should not replace an actual evaluation when symptoms change.
Diagnosis: how heart failure is evaluated
If a clinician suspects heart failure, diagnosis usually includes a mix of:
- History + exam (symptom pattern and changes over time)
- Blood tests (can help detect heart strain and check how other organs are handling fluid balance)
- EKG (checks electrical rhythm and signs of strain/previous injury patterns)
- Chest imaging (can help assess congestion/fluid patterns and other causes of shortness of breath)
- Echocardiogram (ultrasound of the heart) (helps evaluate structure and function)
Sometimes additional testing is needed depending on the situation and the suspected cause.
Treatment: what typically happens by stage
Treatment is individualized, but the big framework often looks like this:
Stage A (risk reduction)
- Control blood pressure, diabetes, cholesterol (when applicable)
- Stop smoking (if relevant)
- Heart-healthy activity and nutrition that you can sustain
- Address sleep issues, alcohol use, weight, and stress patterns (as appropriate)
Stage B (treat heart changes early)
- Ongoing risk reduction
- Medications may be started to reduce strain and prevent progression (your clinician decides what fits)
Stage C (treat symptoms + the underlying cause)
- Medication plans often expand here to control symptoms and reduce flare-ups
- Managing triggers (dietary sodium sensitivity, missed meds, kidney strain, infections, rhythm problems, etc.) becomes a big part of stability
- Follow-up becomes more structured
Stage D (advanced management)
- Closer monitoring
- Specialized therapies (depending on the person’s situation)
- A stronger emphasis on quality of life and preventing repeated severe flare-ups
If you’re reading this and thinking, “I don’t know what stage I’m in,” that’s normal. It’s a reasonable question to ask your clinician directly.
Warning symptoms that shouldn’t wait
If you or a loved one might have heart failure—or you’ve already been told you do—these are warning symptoms that shouldn’t wait:
- Severe or rapidly worsening shortness of breath (especially at rest)
- New or worsening chest pain, pressure, or tightness
- Fainting, near-fainting, severe weakness, or new confusion
- Bluish lips/face or obvious breathing distress
- A very fast or irregular heartbeat with feeling unwell
- Symptoms clearly escalating compared to your usual baseline
If you’re on the fence, it’s reasonable to get evaluated. With breathing and chest symptoms, guessing wrong can get dangerous.
If you’re experiencing new or worsening shortness of breath, swelling, chest discomfort, or a symptom pattern that feels “off”—and you’re in or near Angleton or elsewhere in Brazoria County—it’s reasonable to get evaluated.
At Angleton ER, we’re open 24/7, with board-certified physicians and on-site diagnostics (including imaging and lab testing) to help sort out whether symptoms are heart-related, lung-related, or something else that needs attention.
Educational only. This is not medical advice or a diagnosis. If symptoms are severe, rapidly worsening, or you’re concerned, seek in-person evaluation.
Frequently Asked Questions
What are the 4 stages of congestive heart failure?
Most clinicians refer to Stage A, B, C, and D. Stage A is risk only, Stage B is heart changes without symptoms, Stage C includes current or prior symptoms, and Stage D is advanced heart failure that can be difficult to control.
What is Stage 4 heart failure?
People often say “Stage 4” when they mean Stage D (advanced heart failure) or sometimes NYHA Class IV (symptoms at rest). These are different systems—so it’s worth asking your clinician which one they’re using.
What is Stage C heart failure?
Stage C means there are heart changes and you have symptoms now or you’ve had symptoms in the past. Even if you feel okay today, a prior symptom episode can keep you in Stage C.
What is end-stage heart failure?
“End-stage” is often used informally to describe advanced heart failure (Stage D). It does not automatically tell you “how long” someone has. It signals that symptoms may be hard to control and care may need to be more specialized and more closely managed.
How many stages of heart failure are there?
In the commonly used staging system, there are four stages (A–D). You may also see four NYHA classes (I–IV), which describe symptom limitation rather than disease progression.