If you searched “can heart failure be reversed,” you’re probably not looking for a perfect medical definition.
You’re looking for something simpler—and more personal:
“Is there any way this gets better?”
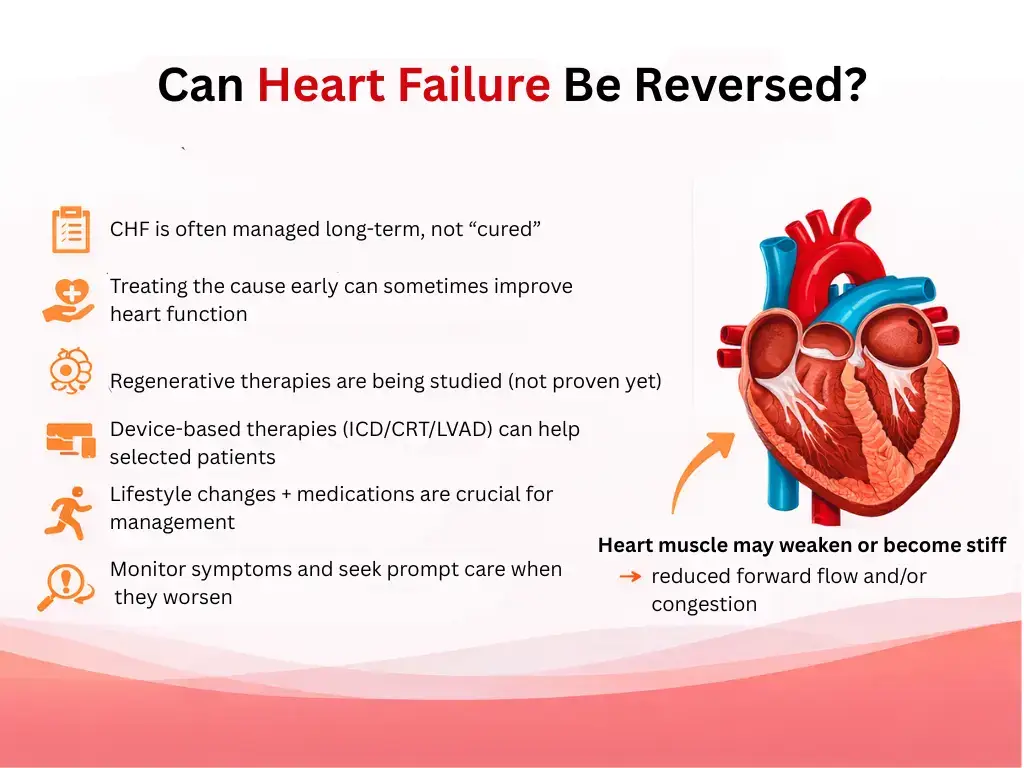
Yes, heart failure can improve in many people with the right treatment and follow-up. And in some cases, heart function can improve dramatically—especially when the underlying cause is identified and treated.
But I’m going to be careful with the word “reversed.” Online, it gets used in a way that can be misleading. Let’s talk about what doctors mean, what improvement can look like, and when symptoms shouldn’t wait.
Educational only. This is not medical advice or a diagnosis. If symptoms are severe, rapidly worsening, or you’re concerned, seek in-person evaluation.
A quick anonymous scenario (what we hear all the time)
Someone comes in and says:
- “I’ve been more winded than normal.”
- “My legs are swelling by the end of the day.”
- “I’m sleeping propped up.”
- “I keep asking myself… is this heart failure? And if it is… am I stuck like this forever?”
That question—“am I stuck?”—is exactly why this article exists.
What “reversible” actually means (in plain language)
“Reversible” doesn’t always mean “cured”
When people ask “can you reverse heart failure,” they usually mean one of these:
- Can my symptoms get better? (less shortness of breath, less swelling, more stamina)
- Can my heart function improve on tests?
- Can I get back to normal life?
All three are possible for many people, but not in the same way for everyone.
There are two different kinds of “getting better”
1) Symptom improvement:
You breathe easier, you retain less fluid, you can do more without feeling wiped out.
2) Heart function improvement:
Your heart looks stronger on imaging (like an echocardiogram), and the overall strain on the heart can decrease.
Sometimes both happen. Sometimes symptoms improve more than the heart function numbers. Sometimes it’s the other way around. The important thing is: improvement is real—and it’s worth pursuing.
Can congestive heart failure be reversed?
People also search “can congestive heart failure be reversed” and “is congestive heart failure reversible.”
“Congestive” often refers to the fluid-backup side of heart failure—fluid in the lungs, swelling in the legs, rapid weight changes from fluid shifts.
That congestion can often be brought under control with treatment. For some people, once the underlying driver is addressed, the heart and fluid balance can stabilize long-term.
But again: “reversed” can mean different things.
- Congestion controlled is a huge win.
- Heart function improved can also happen.
- A permanent cure depends heavily on the cause.
Causes that are more likely to improve (this is where hope gets practical)
Heart failure isn’t one single disease. It’s a final common pathway—many different problems can lead to the same symptom pattern.
Some of those problems are more treatable than others.
High blood pressure strain (a common driver)
If the heart has been pushing against uncontrolled blood pressure for years, treatment and consistent control can reduce strain and, in some cases, allow the heart to recover some function.
Rhythm-related heart failure (like uncontrolled atrial fibrillation)
Certain rhythm problems—especially when fast or irregular over time—can weaken the heart. When the rhythm issue is controlled, heart function can improve in some people.
Valve problems (when addressed)
If a valve issue is significantly contributing to heart strain, addressing it can sometimes lead to meaningful improvement.
Inflammation or certain temporary triggers
Some cases related to inflammation or a clear temporary trigger may improve with time and treatment. Not all—but some.
Lifestyle and medication contributors (the real-world “hidden drivers”)
We also see heart failure symptoms worsen or improve based on:
- medication adherence (not shame—just reality)
- high sodium intake sensitivity
- alcohol use patterns
- sleep issues (including sleep apnea)
- uncontrolled diabetes
- kidney strain
- infections
When these drivers are managed consistently, many people feel noticeably better and have fewer flare-ups.
Symptoms: what “improvement” often looks like in real life
People sometimes expect improvement to feel dramatic. Often it’s quieter:
- you’re less winded walking across the house or parking lot
- you can lie flatter without feeling like you can’t breathe
- your shoes don’t feel tight every evening
- swelling becomes less frequent or less severe
- you stop “saving your energy” all day because you don’t feel as depleted
- your sleep becomes less interrupted by breathing discomfort
- you have fewer sudden “bad days”
If you’re tracking your symptoms and thinking, “Some weeks I’m better, some weeks I’m worse,” that can still be normal—especially early in treatment or during trigger events (like respiratory illness).
Diagnosis: how we tell whether heart failure is improving (without guessing)
If you’re asking “how to reverse heart failure” or “how can heart failure be reversed,” part of the answer is: we monitor what’s changing.
We look at your symptom trend
- How far can you walk compared to last month?
- Are you sleeping flatter?
- Are flare-ups less frequent?
- Is swelling less persistent?
We use testing to confirm what’s happening
Depending on your situation, clinicians may use:
- Echocardiogram (to reassess structure/function over time)
- Blood tests (to monitor strain and organ effects)
- EKG (to watch rhythm issues that can worsen or improve the picture)
- Chest imaging when breathing symptoms shift
The point isn’t to chase a perfect number. The point is to confirm:
- Is your heart under less strain?
- Are we controlling fluid balance?
- Are we addressing the cause?
Treatment: what typically helps (the “getting better” plan)
There isn’t one magic switch. Treatment is usually a combination of:
Treat the driver (the cause)
If blood pressure, rhythm, valve disease, coronary disease, or another underlying issue is driving heart failure, addressing that driver matters.
Medications that reduce strain and help stability
Different medications are used depending on the type of heart failure and your overall health picture. The big idea is:
- reduce the workload on the heart
- improve the heart’s efficiency
- prevent fluid overload flare-ups
- reduce symptom burden
I’m intentionally not listing dosing, thresholds, or “this medicine guarantees recovery,” because that’s not safe or honest. Medication choice is individualized and should be decided with your clinician.
Lifestyle that actually supports recovery (without preaching)
People often search:
- can heart failure be reversed with exercise
- can exercise reverse heart failure
- can weight loss reverse heart failure
Here’s the doctor answer:
- Exercise can help many people with heart failure—but it needs to be appropriate and safe for your condition. The goal is usually steady conditioning, not pushing through symptoms.
- Weight management can help—especially when excess weight is contributing to blood pressure strain, sleep apnea, and metabolic stress.
- The best lifestyle plan is the one you can sustain and the one your clinician says is safe for you.
If exercise makes you severely short of breath, dizzy, faint, or causes chest pressure, that’s not a “push through it” situation. That’s a get evaluated situation.
Prevention: how to reduce flare-ups and protect your progress
Even when heart failure improves, flare-ups can happen. Preventing setbacks often comes down to:
- taking medications as prescribed (again: no shame, just cause-and-effect)
- keeping follow-up appointments (so treatment can be adjusted early)
- watching for symptom drift (your baseline matters)
- being careful with respiratory infections (they can trigger worsening symptoms)
- asking about medications that can worsen symptoms (your clinician can advise)
The goal is not perfection. The goal is stability.
Is heart failure curable?
This is one of the most common (and most loaded) searches:
- is heart failure curable
- is congestive heart failure curable
In many cases, heart failure is treated as a long-term condition. That doesn’t mean “nothing can be done.” It means:
- you may need ongoing management
- you can still improve significantly
- many people live meaningful lives with good symptom control
Sometimes, if the underlying cause is corrected early and effectively, a person can improve to the point where the heart functions much better and symptoms are minimal. But I avoid promising the word “cure” online, because it depends heavily on the cause and the individual medical picture.
Warning symptoms that shouldn’t wait
If you’re wondering whether you’re “safe to watch this,” here are warning symptoms that shouldn’t wait:
- Severe or rapidly worsening shortness of breath, especially at rest
- New or worsening chest pain, pressure, or tightness
- Fainting, near-fainting, severe weakness, or new confusion
- Bluish lips/face or obvious breathing distress
- A very fast or irregular heartbeat with feeling unwell
- Symptoms escalating quickly or clearly different from your baseline
If you’re on the fence, it’s reasonable to be checked. With breathing and chest symptoms, guessing wrong can get dangerous.
If you’re experiencing new or worsening shortness of breath, swelling, chest discomfort, or a fast/irregular heartbeat—and you’re in or near Angleton or elsewhere in Brazoria County—it’s reasonable to get evaluated rather than trying to “wait it out.”
At Angleton ER, we’re open 24/7, with board-certified physicians and on-site diagnostics (including lab services and CT/X-ray/ultrasound imaging) to help assess urgent symptoms when time matters.
Educational only. This is not medical advice or a diagnosis. If symptoms are severe, rapidly worsening, or you’re concerned, seek in-person evaluation.
Frequently Asked Questions
Can heart failure be reversed?
Heart failure can often improve with treatment, and in some cases heart function can improve significantly—especially when the underlying cause is identified and managed. “Reversed” can mean different things, so it’s best to talk with your clinician about what improvement looks like in your specific case.
Can congestive heart failure be reversed?
“Congestive” refers to fluid backup. Fluid-related symptoms can often be brought under control, and some people experience major symptom improvement when treatment is consistent and triggers are addressed.
Is heart failure reversible?
Sometimes. Some causes are more treatable than others, and improvement depends on the underlying driver, how early treatment starts, and how consistently the plan is followed.
Is congestive heart failure reversible?
Congestion can often improve with treatment. Whether heart function itself improves depends on what’s causing the heart failure and how well it responds to therapy.
Can heart failure be reversed with exercise?
Exercise can help many people with heart failure, but it needs to be safe and appropriate for your condition. If exercise triggers severe shortness of breath, dizziness, fainting, or chest pressure, you should be evaluated.
Can weight loss reverse heart failure?
Weight loss can reduce strain on the heart in some people, especially when excess weight is contributing to blood pressure issues, sleep-disordered breathing, or metabolic stress. It’s not a guarantee, but it can be a meaningful part of improvement for the right person.