If you searched “what are the symptoms of heart failure,” you’re probably trying to answer one question:
“Is this something I can watch… or something I shouldn’t ignore?”
That’s a fair question. In real life, heart failure symptoms don’t always show up like a movie scene. Often, they show up as small changes that don’t seem connected—until they start stacking up.
Before we go any further, here’s the steady truth we want you to hold onto:
- Many heart failure symptoms overlap with other conditions (like asthma/COPD, pneumonia, anemia, anxiety, medication side effects, and more).
- What matters most is pattern + change—especially if symptoms are new, worsening, or affecting your breathing.
Educational only. This is not medical advice or a diagnosis. If symptoms are severe, rapidly worsening, or you’re concerned, seek in-person evaluation.
If you’re here, you’re probably trying to make sense of a symptom pattern
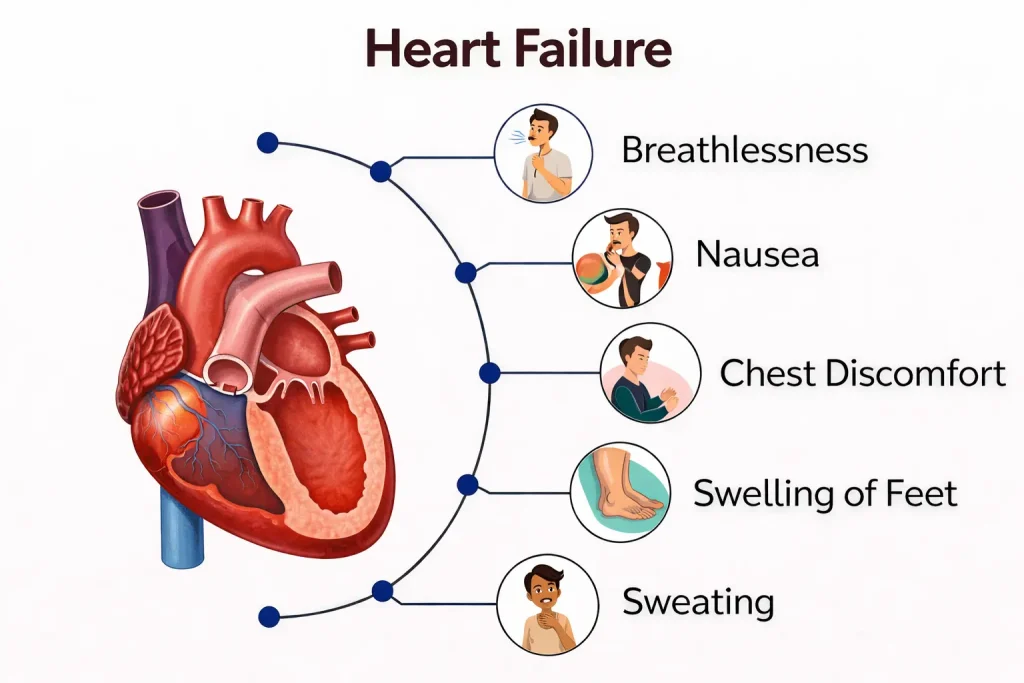
Heart failure symptoms tend to fall into two buckets:
- “Not enough forward flow” — the body isn’t getting what it needs as efficiently, so you feel worn out or winded.
- “Backup / congestion” — fluid builds up where it shouldn’t, especially in the lungs and legs.
That’s why some people describe heart failure symptoms as:
- breathing changes
- swelling
- fatigue that doesn’t match their day
- a cough or “chest congestion” feeling
- a drop in stamina that feels out of proportion
Now let’s make this human and practical.
A quick anonymous scenario (the kind we see all the time)
A patient comes in from Brazoria County and says something like:
“I’m not sick-sick… I just can’t catch my breath like I used to. I’m sleeping propped up, my ankles are swollen, and I’m exhausted doing normal stuff.”
They don’t come in asking for a label. They come in asking for clarity.
In those situations, we’re thinking about two things at once:
- What’s the most dangerous thing this could be (and how do we not miss it)?
- If it’s heart failure or fluid overload, what’s driving it and how do we stabilize it safely?
This article is meant to help you recognize patterns—not to diagnose yourself online.
The most common heart failure symptom patterns we hear (in real-life language)
Shortness of breath (especially when it’s “new for you”)
This is the #1 reason many people seek care.
Heart failure-related shortness of breath often shows up as:
- getting winded doing your usual activities (walking, stairs, chores)
- needing to pause more than normal to catch your breath
- feeling worse when lying flat
- waking up at night feeling like you need to sit up to breathe
- feeling like you “can’t get a full breath,” even without wheezing
not all shortness of breath is heart failure. But if your breathing is changing, worsening, or limiting your day, it’s worth being evaluated—especially if you also notice swelling or fatigue.
A practical question we ask ourselves
“Is this person short of breath at rest, or getting worse fast?”
That’s the difference between “let’s look into this” and “this shouldn’t wait.”
Fatigue and reduced stamina
People often don’t call it fatigue. They call it:
- “I feel heavy.”
- “I’m wiped out after small things.”
- “I’m sleeping but not recovering.”
When the heart can’t keep up with the body’s needs efficiently, your muscles and organs may feel it first as stamina loss. The tricky part is that fatigue also has many non-heart causes—so we look for fatigue that pairs with other changes, like shortness of breath or swelling.
Swelling in the legs, ankles, or feet (and sometimes the belly)
Swelling can show up as:
- sock lines that suddenly leave deeper marks
- shoes that feel tighter by evening
- ankles that look puffy
- a sense of heaviness in the legs
Sometimes people notice a “puffiness” that isn’t just weight gain. That’s an important distinction. Fluid shifts can happen quickly in some conditions, and swelling paired with breathing changes is a pattern we take seriously.
Cough or “chest congestion” that doesn’t fit a typical cold
Some people experience:
- a persistent cough
- a congested feeling in the chest
- symptoms that seem worse when lying down
This can get mistaken for allergies or a lingering respiratory infection. And sometimes it truly is respiratory. But when a cough shows up alongside new shortness of breath, swelling, or reduced stamina, we widen the lens.
Reduced appetite, bloating, or feeling full quickly
Not everyone realizes this can be part of fluid shifts. Some people say:
- “I’m not eating much, I feel full fast.”
- “My stomach feels tight or bloated.”
- “I feel swollen all over.”
Again, this symptom can come from many causes. But when it’s part of a cluster (especially with swelling and breathing changes), it becomes more meaningful.
Symptoms that often get mistaken for “something else”
This is one of the biggest reasons people delay care: they try to make symptoms fit a simpler explanation.
“It’s probably anxiety”
Anxiety can absolutely create real physical symptoms: chest tightness, fast heartbeat, shortness of breath, sweating, nausea. We never dismiss that.
But here’s what changes urgency:
- symptoms that are new, worsening, or happening at rest
- symptoms paired with fainting, confusion, blue lips/face, or chest pressure
- a sense of being “seriously unwell” that you can’t explain
If you’re unsure, it’s reasonable to get evaluated—because guessing wrong with breathing and chest symptoms is a risk most people don’t want to take.
“It’s probably a cold”
Respiratory infections are common. But we get concerned when:
- shortness of breath is escalating quickly
- breathing feels difficult even when you’re not coughing much
- you can’t lie flat comfortably
- symptoms are not behaving like your usual colds
“It’s probably weight gain”
Weight changes can be normal. But sudden changes paired with swelling or breathlessness deserve a closer look. We’re not talking about appearance—we’re talking about function and how you feel.
Why heart failure symptoms happen (simple physiology, no numbers)
When heart failure symptoms show up, it’s usually one (or both) of these dynamics:
Forward-flow problem: less efficient delivery
If your heart isn’t pumping forward effectively, your body may respond with:
- fatigue
- reduced stamina
- lightheadedness
- faster heart rate with mild activity
Backup/congestion problem: fluid buildup
If blood isn’t moving forward as efficiently, pressure can back up and fluid can accumulate:
- lungs → shortness of breath, “congestion” feeling
- legs/ankles → swelling
- abdomen → bloating, appetite changes
Body stress response: the system compensates
Your body tries to help by adjusting hormones, fluid balance, and circulation. This is part of why symptoms can fluctuate and why “baseline” matters.
When we’re more concerned (trend-based, not threshold-based)
We don’t need a perfect internet checklist to decide if symptoms matter. We look at trajectory.
We’re more concerned when symptoms are getting worse quickly
Examples:
- you’re noticeably more short of breath than you were a day or two ago
- swelling is increasing rapidly
- stamina has dropped suddenly
We’re more concerned when symptoms happen at rest
If you’re short of breath while sitting still, or you can’t speak comfortably because breathing is hard, that is not something to “ride out” at home.
We’re more concerned when symptoms cluster with “system alarms”
Chest pressure, fainting, confusion, blue lips/face, or a very fast/irregular heartbeat with feeling unwell—those are not “wait and see” symptoms.
Warning symptoms that shouldn’t wait
If you have possible heart failure symptoms—or you’ve been told you have heart failure—these are warning symptoms that shouldn’t wait:
- Severe or rapidly worsening shortness of breath, especially at rest
- New or worsening chest pain, pressure, or tightness
- Fainting, near-fainting, severe weakness, or new confusion
- Bluish lips/face or obvious breathing distress
- A very fast or irregular heartbeat with feeling unwell
- Symptoms escalating quickly or clearly different from your baseline
If you’re on the fence, it’s reasonable to be checked. We would rather evaluate you early than meet you later when you’re in a worse spot.
If you’re experiencing shortness of breath, new swelling, chest discomfort, or symptoms that feel like they’re getting worse—and you’re in or near Angleton or elsewhere in Brazoria County—it’s reasonable to get evaluated. If you’re not sure what you’re feeling, we can help you sort out what’s going on and whether it’s heart-related, lung-related, or something else that needs attention.
Educational only. This is not medical advice or a diagnosis. If symptoms are severe, rapidly worsening, or you’re concerned, seek in-person evaluation.
Frequently Asked Questions
What are the symptoms of heart failure?
Common heart failure symptom patterns include shortness of breath (especially with activity or lying flat), fatigue and reduced stamina, swelling in the legs/ankles, and sometimes cough or a congested feeling. Symptoms vary—what matters most is new or worsening change.
What are the symptoms of congestive heart failure?
Congestive heart failure often refers to symptoms related to fluid backup (“congestion”), such as shortness of breath, swelling, and rapid changes in exercise tolerance. Many people also feel unusually tired or “heavy.”
What does heart failure feel like?
People describe it as getting winded doing normal activities, needing to sleep propped up, feeling wiped out with small tasks, or noticing swelling that wasn’t there before. The experience isn’t identical for everyone.
Is coughing a sign of heart failure?
A cough can be part of heart failure—especially if it clusters with shortness of breath, swelling, or worsening stamina. But cough has many causes, so context and change are important.
Can heart failure cause nausea or indigestion-like symptoms?
Some people experience nausea or a “not-right” stomach feeling during cardiac strain, but those symptoms are not specific. If nausea is paired with chest pressure, sweating, shortness of breath, or a sense of being seriously unwell, urgent evaluation is reasonable.
When should I go to the ER for heart failure symptoms?
If you have warning symptoms that shouldn’t wait—severe breathing trouble, new chest pressure/pain, fainting, confusion, blue lips/face, or rapidly worsening symptoms—seek urgent evaluation.