If you searched “how to treat congestive heart failure,” there’s a good chance you’re not looking for trivia. You’re looking for something steadier than internet noise — a clear plan, in plain language, so you can breathe a little easier (sometimes literally).
Here’s what we tell patients in real life:
- CHF is serious, but it’s often treatable and manageable.
- Treatment isn’t one magic fix. It’s usually a combination of the right meds, the right daily habits, and catching flare-ups early.
- If symptoms feel like they’re getting worse fast, don’t try to “tough it out.” That’s the moment for evaluation.
Educational only. This is not medical advice or a diagnosis. If symptoms are severe, rapidly worsening, or you’re concerned, seek in-person evaluation.
What “treating CHF” actually means
“Congestive heart failure” doesn’t mean your heart “stopped.” It means your heart isn’t keeping up with your body’s needs the way it should, and your body may hold onto fluid. That fluid backup is what drives a lot of the symptoms people notice.
When we talk about CHF treatment, we’re usually targeting two goals:
- Reduce congestion (help you breathe easier, reduce swelling, improve stamina)
- Reduce strain on the heart over time (so symptoms flare less often and day-to-day life is more stable)
A quick anonymous scenario
A person from Brazoria County tells us:
- “I get winded walking from the car.”
- “I can’t lie flat comfortably.”
- “My legs look puffy by evening.”
- “I thought it was stress… but it’s getting worse.”
They’re not trying to become their own cardiologist. They’re trying to answer:
“Is this urgent — and what can I do next?”
Symptoms people notice
CHF symptoms can be subtle at first, and that’s part of what makes it stressful.
Common ways people describe it:
- Shortness of breath
- with activity, when lying down, or waking up breathless
- Swelling
- ankles/feet/legs, sometimes hands or belly “bloating”
- Fatigue that doesn’t match your day
- “I feel wiped out doing normal stuff”
- Cough or chest congestion
- especially if fluid is backing up toward the lungs
- Rapid weight change
- not “fat gain,” but fluid changes (this is why clinicians often ask you to watch trends)
These symptoms can overlap with other conditions, so the goal isn’t self-diagnosis — it’s recognizing when something needs a real evaluation.
Causes & who is at risk
CHF usually develops because the heart has been under strain or has been injured over time — and sometimes a new event “tips it over.”
Common contributors include things like:
- Long-term high blood pressure
- Coronary artery disease (reduced blood flow to heart muscle)
- Prior heart attack or heart muscle weakness
- Valve problems
- Irregular heart rhythms
- Uncontrolled diabetes, kidney disease, lung disease, and other chronic conditions that raise overall strain
And then there are triggers that can make symptoms suddenly worse (even in someone already diagnosed), such as:
- infections and illnesses
- missed meds or medication changes
- fluid shifts
- worsening blood pressure control
- new rhythm problems
If CHF is on the table, we don’t just ask “do you have heart failure?”
We ask: “What’s driving it — and what’s making it worse right now?”
How CHF is diagnosed (the tests that clarify what’s going on)
CHF isn’t diagnosed from one single clue. It’s usually a combination of:
- your symptoms and medical history
- a physical exam (listening to lungs/heart, checking swelling, oxygen status, etc.)
- tests that help confirm heart strain and fluid overload, and rule out other causes
- EKG/ECG (rhythm and heart strain clues)
- Blood tests
- clinicians may check markers that rise with heart strain and see how kidneys/liver are doing
- Chest X-ray
- can show signs of fluid in the lungs or other chest issues
- Echocardiogram (heart ultrasound)
- helps evaluate how the heart is pumping and filling
- Additional testing
- sometimes stress testing or other imaging, depending on what’s suspected
If you’re reading this because symptoms are changing quickly, the key point is:
Don’t gamble on guessing. CHF and several other conditions can feel similar early on.
Treatment options for congestive heart failure (the plan that actually helps)
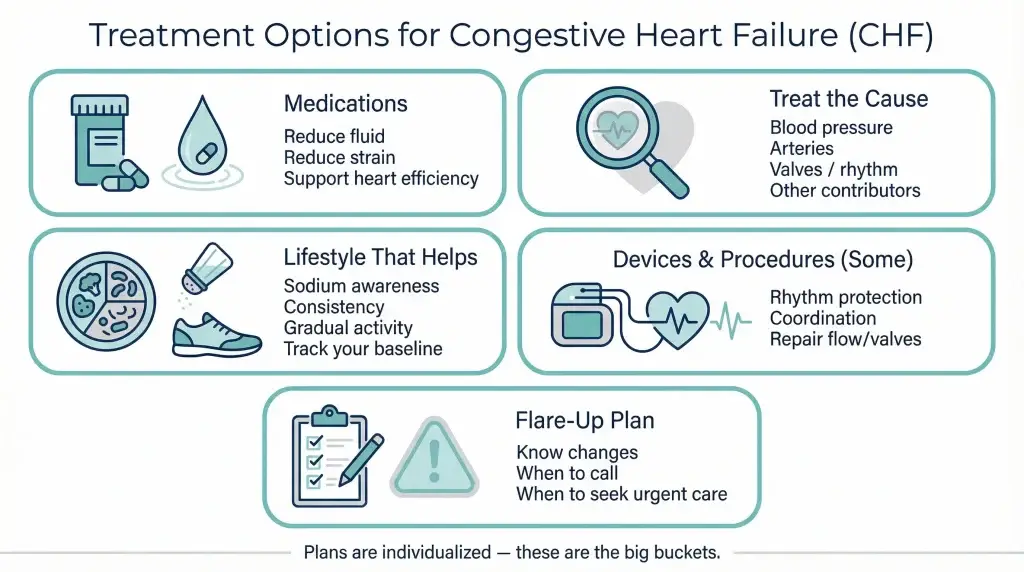
Treatment is individualized — but the “big buckets” are consistent.
Medications (often more than one, for different reasons)
CHF treatment frequently involves a combination of medicines because each class targets a different part of the problem.
Depending on your situation, clinicians may use medications that help:
- reduce extra fluid (to relieve congestion and swelling)
- relax blood vessels / reduce strain on the heart
- slow heart rate and improve heart efficiency
- stabilize hormone pathways that worsen CHF over time
- support heart and kidney function in ways that reduce hospitalizations for some patients
Two practical notes we repeat a lot:
- Do not start/stop CHF meds on your own. Even “small changes” can matter.
- If side effects show up, don’t just quit. Tell your clinician — there are often alternatives.
Treat the underlying cause (this is where progress happens)
CHF management is much stronger when we address what’s driving it. That could mean treating:
- blood pressure issues
- blocked coronary arteries
- valve problems
- rhythm problems (like atrial fibrillation)
- thyroid issues, kidney strain, or other contributors
This is one reason we don’t love “one-size-fits-all” internet answers.
The best CHF treatment depends on what caused it.
Lifestyle changes that actually matter (without turning your life into a punishment)
Lifestyle isn’t about perfection — it’s about reducing the most common forces that worsen CHF.
Often-helpful habits include:
- Sodium awareness
- CHF and salt don’t get along for many people; processed foods are a common issue
- Medication consistency
- the “best” plan doesn’t help if it’s taken randomly
- Activity that’s appropriate for your symptoms
- many people do better with gradual, consistent movement than with overdoing it then crashing
- Monitoring your baseline
- noticing earlier when swelling, breathing, or stamina is changing
If you’ve never lived with CHF symptoms, it’s easy to underestimate how real it is. We don’t.
We’d rather help you build a sustainable plan than scare you into doing nothing.
Devices and procedures (for some patients, not all)
Some people benefit from implanted devices or procedures when CHF is more advanced or when rhythm risk is higher.
Depending on your case, this can include:
- devices that correct dangerous rhythms
- devices that help coordinate how the heart beats
- procedures that repair structural problems (like valves) or improve blood flow
You don’t need to memorize device names to understand the point:
For some patients, “treating CHF” includes more than meds — and that’s not a failure. It’s a strategy.
“Flare-up” planning (this is how many ER visits are prevented)
A lot of CHF ER visits happen because symptoms quietly worsen… until they don’t feel quiet anymore.
A flare-up plan usually means:
- knowing what symptom changes matter for you
- knowing when you should call your clinician
- knowing when you should seek urgent evaluation instead of waiting
Which brings us to the part we never soften:
Prevention: lowering the chance of CHF flare-ups
CHF isn’t always preventable once it’s established — but flare-ups are often reducible.
Things that commonly help reduce “backslides”:
- taking medications as prescribed
- keeping follow-up appointments (even when you feel “okay”)
- addressing blood pressure, diabetes, kidney strain, and rhythm problems consistently
- avoiding extreme swings in daily habits (overdoing activity, major diet swings, missed meds)
- treating infections early (because illness can trigger worsening symptoms)
The goal isn’t “never have a bad day.”
The goal is: fewer emergencies, more stability, and earlier action when things change.
Warning symptoms that shouldn’t wait (when ER evaluation is reasonable)
If CHF is possible — or already diagnosed — these are warning symptoms that shouldn’t wait:
- Severe or rapidly worsening shortness of breath, especially at rest
- New or worsening chest pain, pressure, or tightness
- Fainting, near-fainting, new confusion, or severe weakness
- Bluish lips/face or obvious breathing distress
- A very fast or irregular heartbeat and you feel unwell
- Symptoms escalating quickly or feeling different from your usual baseline
If you’re experiencing symptoms like these and you’re in or near Angleton (or elsewhere in Brazoria County), it’s reasonable to get evaluated.
If your breathing is changing, swelling is worsening, or you feel like something is sliding the wrong direction — and you’re in/near Angleton — it’s reasonable to be checked. Our team at Angleton ER is open 24/7, with board-certified physicians and on-site diagnostics (lab testing and imaging) available when needed.
Educational only. This is not medical advice or a diagnosis. If symptoms are severe, rapidly worsening, or you’re concerned, seek in-person evaluation.
Frequently Asked Questions
Is congestive heart failure treatable?
Yes — CHF is often treatable and manageable, especially when the underlying cause is addressed and symptoms are monitored early. Treatment is usually a combination of medications, daily habits, and follow-up care.
How do you treat congestive heart failure?
Most CHF treatment plans include:
medications to reduce fluid and strain on the heart
treating the root cause (blood pressure, blocked arteries, valve issues, rhythm problems, etc.)
lifestyle changes that support stability
sometimes devices or procedures, depending on severity and risk
What is the best treatment for congestive heart failure?
There isn’t one “best” universal treatment. The best plan is the one matched to your type of heart failure and what caused it, and adjusted based on how you respond.
Can heart failure be reversed?
Sometimes heart function and symptoms can improve significantly, especially if the underlying cause is treatable and the plan is followed closely. But avoid anyone promising a guaranteed “reversal” online — CHF is too individualized for that.
When should someone with CHF go to the ER?
If symptoms are severe, rapidly worsening, or include warning symptoms that shouldn’t wait (like severe shortness of breath, chest pain, fainting, confusion, blue lips/face, or feeling seriously unwell), urgent evaluation is appropriate.